History
In the mid1990’s H. Theodore Harcke, MD, a pediatric radiologist at Nemours/A.I. duPont Hospital for Children and Richard Henderson, MD, PhD, a pediatric orthopedic surgeon from UNC/Chapel Hill thought about the problems encountered in measuring bone density by DXA in patients with physical disabilities. These problems include:
- joint contractures
- dislocated hips
- inability to hold still during the scan (movement disorders)
- inability to lie flat on the scanning table
- presence of metallic hardware (orthopedic rods/clips/pins)
- presence of other artifacts (feeding tubes, shunts, pumps)
Most of these problems affect the accuracy and validity of DXA measures obtained at the typical sites measured by DXA including the total body, lateral spine, and proximal femur (hip). They proposed scanning the knee (distal femur) in the lateral view by DXA because it is:
- easily obtained – comfortable side-lying position
- quick scan time – less than 30 seconds
- most clinically relevant site to measure in people who are non-weight bearing – most low-energy fractures experienced in the non-ambulatory population are of the lower extremities, particularly of the distal femur
- works well for people with positioning limitations (tight joints/contractures) and indwelling artifacts (rods, tubes, etc) that would affect other DXA results of other body sites.
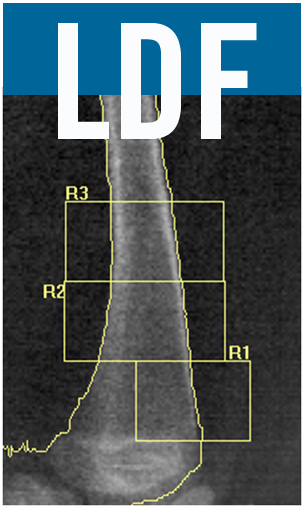
The first paper introducing the LDF was published in 1998:
The proposed Regions of Interest (ROIs) attempted to examine cortical vs. trabecullar bone.
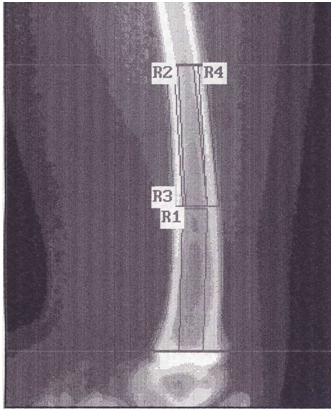
It was later decided that creation of these ROIs was cumbersome with the software available at the time and an easier approach for analysis was developed and introduced with the first set of published norms in 2002.
The ROIs utilizing this analysis technique allow for evaluation of three different combinations of bone: R1 contains primarily metaphyseal or trabecullar bone; R2 contains metadiaphyseal bone with a mix of trabecullar and cortical bone; R3 contains primarily diaphyseal or cortical bone. The norms presented in the 2002 paper were acquired on pencil-beam DXA systems and included values from 256 boys and girls aged 3 - 18 years of Caucasian race. The norms were calculated employing prediction equation statistical methodology.
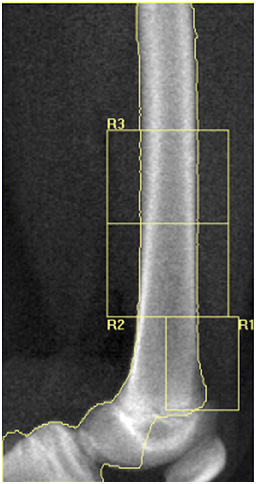
With the advent of fan-beam systems, it became necessary to collect and make available norms acquired on fan-beam systems for valid comparison purposes. The positioning and ROIs remained the same. Normative values based on fan-beam norms became available in 2009:
These normative values were acquired on 821 boys and girls of black and Caucasian race and include the ages of 6 - 18 years. The LMS method was used as the statistical method for the calculation of these norms. Because of the differing sample sizes and different statistical models used for calculation of normative values, there is no comparison or conversion factor between the two normative databases (pencil beam vs. fan beam norms). The 2009 LDF norms (Zemel) are currently in use for the LDF. Normative values below the age of 6 years and above 18 years have not yet been determined.
To date, nearly every institution using the LDF DXA technique has sought and received onsite, hands-on training by one lead technologist, followed by quality assurance assessments of technique with troubleshooting support. Over thirty institutions from around the world (most in the US) have had this training. In addition, one pharmaceutical company developed scanning instructions in consultation with the team who originated the technique for use in a clinical trial of a bisphosphonate where the LDF is an outcome measure. While most institutions use the LDF as a part of clinical assessment of patients, a few institutions reserve the LDF DXA for research purposes only.